Book Appointment Now

Stem Cell Therapy in Latin America: Patient Guide (Non-Transplant)
Stem cell therapy offers a potential way to support repair of tissues affected by disease or injury. In recent years, many Americans and Europeans have looked to Latin America for these non-transplant regenerative treatments—largely due to lower costs, faster access, and broader availability than at home.
This guide explains what to know before pursuing stem cell therapy (non-transplant) in Latin America. We cover why people travel, the main destinations (Panama, Colombia, Mexico), sample prices, what treatment visits look like, and the safety checks that matter. Because many uses are still experimental and rules differ by country, having clear, evidence-based information is essential.
Note: This article focuses on non-transplant stem cell therapy (e.g., mesenchymal stem cell treatments). For information about stem cell transplant (HSCT/BMT), see our related guide linked once below.
Why Latin America Is Emerging in Regenerative Medicine
Latin America draws patients for lower costs, faster access, and broader availability of non-transplant therapies—balanced by the need for careful clinic vetting.
Cost Advantages
Patients often save 50–70% versus U.S. prices due to lower operating costs, favorable exchange rates, and competitive medical tourism markets.
Regulatory Environment
Agencies such as COFEPRIS (Mexico), INVIMA (Colombia), and MINSA (Panama) may permit certain non-transplant uses considered experimental elsewhere—offering faster access but requiring stronger due diligence.
Investment and Infrastructure
Modern clinics and concierge services have expanded for international patients—raising convenience while making clinic screening essential to avoid hype.
Physician Expertise
Reputable centers disclose physician licensing, training, and procedure volumes; prioritize clinics that make credentials and protocols transparent.
Accessibility
Mexico is a short flight for many North Americans; Panama and Colombia also have strong air links. Many clinics coordinate transport and lodging.
What is Stem Cell Therapy?
Non-transplant therapy uses stem cells to modulate inflammation or support tissue repair. Understanding cell types and sources helps you evaluate protocols.
What Are Stem Cells?
They self-renew and can differentiate into multiple cell types (e.g., muscle, blood, nerve).
Where Stem Cells Come From

- Embryonic: Highly versatile; ethically and legally restricted.
- Adult: Bone marrow/adipose; MSCs commonly used to modulate inflammation.
- iPSCs: Reprogrammed adult cells; largely experimental clinically.
- Perinatal: Umbilical cord blood/tissue; cord blood has established uses in transplant settings.
Your Cells vs. Donor Cells
- Autologous: Your cells; lower rejection risk; requires harvesting; potency varies by age/health.
- Allogeneic: Donor cells (often umbilical cord); readily available; immune reactions usually low with MSCs but possible.
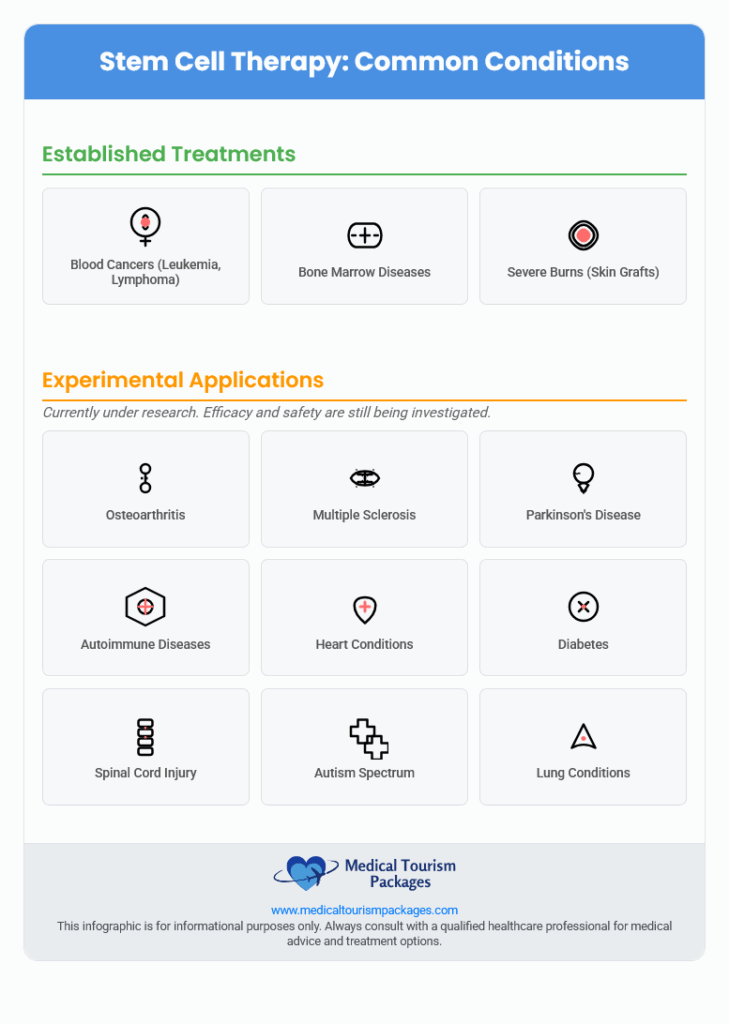
Proven vs. Experimental Uses
Proven: Narrow indications (e.g., bone marrow use for blood disorders within transplant care; skin grafting for severe burns).
Experimental: Osteoarthritis, neurological, autoimmune, cardiometabolic, and anti-aging uses lack large, high-quality trials. Treat claims critically.
Stem Cell Therapy vs. Transplant—what’s the difference?
This page covers non-transplant therapies (e.g., MSC infusions/injections) aimed at symptom relief or functional support for orthopedic, autoimmune, or neurological conditions. If you need information on transplant (HSCT/BMT) for blood cancers/genetic disorders, read: Stem Cell Transplant in Latin America.
Who is (and isn’t) a candidate?
- Often suitable: Stable orthopedic pain, select autoimmune or neuro conditions, realistic goals, willingness to follow rehab/lifestyle plans.
- Usually not suitable: Active cancer/recent malignancy, uncontrolled infection, pregnancy/breastfeeding, severe bleeding disorders, decompensated organ failure, or inability to adhere to follow-up.
- Before treatment: Expect imaging or specialist clearance for joints/spine/neuro protocols.
Top Destinations for Stem Cell Therapy
Three countries stand out for infrastructure and access: Panama, Colombia, and Mexico.
Quick comparison:
| Feature | Panama | Colombia | Mexico |
|---|---|---|---|
| Main Regulatory Body | Ministry of Health (MINSA) | National Institute of Food and Drug Monitoring (INVIMA) | Federal Commission for Protection Against Sanitary Risks (COFEPRIS) |
| Some Notable Clinics | Stem Cell Institute Panama, PCT Panama | BioXcellerator, TRT Colombia | R3 Stem Cell International, Giostar Mexico |
| General Cost Range | $5k–$25k | $3k–$15k | $1.5k–$15k |
| Accreditations to Look For | JCI (some hospitals), ISO, GMP | ISO, cGMP, GCP, JCI (some hospitals) | COFEPRIS Certification, JCI (some hospitals) |
Panama: A Hub for Advanced Therapy
Known for international patient services and modern facilities; verify each clinic’s protocol, lab quality, and evidence for your indication.
Leading Clinics
Examples include Stem Cell Institute Panama (umbilical cord–derived cells) and PCT Panama; Hospital Punta Pacífica (JCI-accredited) offers regenerative services. Always verify claims independently.
Rules and Regulations
MINSA oversees therapies; JCI indicates hospital-level quality systems but not treatment efficacy for experimental uses.
What Patients Experience
Concierge support (airport transfers, hotel coordination) is common; rely on third-party evidence rather than marketing outcomes.
Transplant-specific guide: Stem Cell Transplant in Latin America
Colombia: Innovation and Affordability
Offers comparatively lower prices with growing medical tourism hubs in Medellín and Bogotá; review protocols and follow-up plans carefully.
Leading Clinics
Providers such as BioXcellerator market cord-derived MSCs and emphasize ISO/cGMP/GCP systems; JCI-accredited hospitals offer broader specialty support.
Rules and Regulations
INVIMA regulates tissue banking, donor screening, and research; advertising claims for unproven uses are restricted.
What Patients Experience
Strong value and developing aftercare networks; confirm detailed protocols, dosing, and follow-up cadence before booking.
For a broader view, see our Colombia Destination Overview.
Mexico: Accessibility and Established Medical Tourism
Most accessible for U.S./Canada; large cost savings; many clinics in border/resort cities—scrutinize each protocol’s quality and regulatory status.
Leading Clinics
Examples: R3 Stem Cell International, Giostar Mexico, Progencell (Tijuana). COFEPRIS certification matters—still verify dosing, lab reports, and consent.
Rules and Regulations
COFEPRIS regulates facilities/protocols; some non-transplant uses available here may be limited to trials in the U.S.—request documentation.
What Patients Experience
Major cost savings and straightforward travel; many clinics assist with logistics and bundled lodging.
Cost Comparison: U.S. vs. Latin America
Prices vary by indication, cell source, dose, delivery method, and clinic. Typical ranges are below U.S. levels.
Examples:
- Knee Osteoarthritis: U.S. $5,000–$12,000 • Colombia $3,000–$6,000 • Mexico $1,500–$3,100
- Autoimmune/Neurological programs: U.S. $20,000–$50,000+ • Colombia $5,000–$15,000 • Mexico $7,000–$15,000
- Wellness/Anti-aging: U.S. $5,000–$10,000+ • Colombia $2,500–$5,000 • Mexico ~$500–$6,500
This table summarizes sample estimates:
| Condition | US Cost | Panama Cost | Colombia Cost | Mexico Cost |
|---|---|---|---|---|
| Knee Osteoarthritis | $5,000–$12,000 | $5,000–$25,000 | $3,000–$6,000 | $1,500–$3,100 |
| Autoimmune/Neurological Programs | $20,000–$50,000+ | $5,000–$25,000 | $5,000–$15,000 | $5,500–$15,000 |
| Wellness/Anti-aging | $5,000–$10,000+ | $5,000–$25,000 | $2,500–$5,000 | ~$500–$6,500 |
Estimates are based on clinic-reported ranges; always confirm what’s included.
Why it’s cheaper:
- Lower facility and administrative costs
- Lower local salaries
- Exchange-rate advantages
- Competitive medical tourism markets
- Less costly regulatory pathways for experimental therapies
What’s typically included: consultations, basic testing, harvesting (if autologous) or donor cells, the procedure(s), and limited follow-up. Travel, hotels, meals, and management of complications may be extra.
What your quote should include (to compare apples to apples)
- Cell source (autologous vs. donor), dose (viable cells per kg/joint), session count, and route (IV/intra-articular/intrathecal)
- Lab reports: sterility, endotoxin, mycoplasma, viability %, MSC markers, passage number
- Imaging/labs, consumables (e.g., image-guided injections), and medications on treatment days
- Follow-up schedule and telehealth access
- What’s excluded (complications, hospital transfers, lodging)
What to Expect During Your Medical Trip
Most programs follow a predictable flow from remote review to onsite treatment and structured follow-up.
Initial Consultation and Evaluation
- First contact: Online form or call
- Record review: Candidacy screening
- Consultation: Protocol, benefits/risks, pricing
- Plan: Cell source, dose, delivery, sessions, schedule
- Booking: Costs, payment, itinerary
The Treatment
- Pre-checks: Final exam and labs
- Administration:
- IV for systemic indications
- Image-guided joint injections for orthopedic issues
- Intrathecal (spinal) for select neuro protocols
- Other routes as protocolled
Recovery and Follow-up
- After treatment: Rest at hotel; limited downtime for injections
- Return travel: Many itineraries finish within 2–5 days
- Follow-up: Remote check-ins (calls/emails/video)
Recommended follow-up cadence
- 1–2 weeks: Safety/adverse events
- 1 month: Early response; adjust rehab
- 3 months: Primary outcomes (pain/function scores)
- 6 months: Progress; discuss adjuncts (e.g., PT/PRP)
- 12 months: Long-term outcomes/next steps
Combining Treatment and Tourism
Plan leisure before treatment or after adequate recovery; prioritize rest immediately post-procedure per your clinician’s advice.
Safety and Legal Considerations
Reduce risk by verifying facility standards, lab quality, dosing clarity, and informed consent before committing.
Clinic Accreditation and Standards
- JCI: Hospital-level quality systems (not proof of specific therapy efficacy)
- ISO: Quality management
- GMP: Cell processing (sterility, potency, purity)
- GCP: Human research standards
- National: e.g., COFEPRIS (Mexico)
How clinics source, test, and dose cells
- Source: Autologous vs. donor (umbilical cord); request donor screening panel results.
- Manufacturing: GMP facility with batch Certificates of Analysis (sterility, endotoxin, mycoplasma, viability).
- Potency & passage: Ask for viability %, MSC markers, and culture passage number.
- Dose clarity: Viable cells per kg (or per joint/route) > marketing “billions.”
- Chain of custody: Documented cold-chain and time from thaw to administration.
Treatment Protocols and Risks
- Informed consent: Procedure details, evidence (or lack), experimental status, risks/benefits, alternatives, costs, patient rights—in your language, in advance.
- Known risks: Infection, immune reactions, unwanted tissue growth, ocular injury (for eye injections), clots, organ injury, worsening symptoms, rare fatalities.
- Oversight varies: COFEPRIS/INVIMA/MINSA requirements differ from U.S./EU standards—verify documentation.
Clinic red flags to avoid
- “Cure-all” claims or identical protocol for many unrelated diseases
- Refusal to share lab reports, dosing, or passage/viability data
- Very high cell counts with no viable cell data
- Pressure to pay before medical review or no consent window
- No plan for complications or lack of nearby hospital backup
Patient Rights and Legal Recourse
Cross-border malpractice claims are complex and costly, and enforcement can be difficult. Factor this into your decision-making and document everything.
For comparative legal context, see the Library of Congress – Stem Cell Research Regulations.
What results to expect (and when)
- Orthopedic (e.g., knee OA): Aim for pain/function changes over 3–6 months with structured physical therapy.
- Neurological: If improvements occur, they are typically gradual over 6–12+ months and variable.
- Autoimmune: Goals include symptom control and fewer flares alongside specialist care.
- No guarantees: Most non-transplant uses remain experimental; responses vary.
FAQs About Stem Cell Therapy in Latin America
Answers to common questions about non-transplant stem cell therapy in the region:
What conditions can stem cell therapy treat?
Proven uses are limited (e.g., certain blood disorders within formal transplant care; skin grafting for severe burns). Most other uses are experimental—review evidence quality, realistic outcomes, and risks with your provider.
Is stem cell therapy safe in Latin America?
Safety depends on clinic, protocol, and indication. Look for GMP processing with batch reports, qualified physicians, dosing clarity, and robust informed consent. Be wary of universal “cure” claims or minimized risks.
How much does stem cell therapy cost in Colombia or Panama?
Typical ranges: Panama $5,000–$25,000; Colombia $3,000–$15,000. Request a written quote stating cell source, viable dose, session count, follow-up, and exclusions.
How long does recovery take?
Joint injections often have minimal downtime; systemic or intrathecal protocols may need activity limits. Confirm specific restrictions and milestones with your clinic.
How do I find a trustworthy clinic abroad?
Verify physician licensing, GMP/GCP adherence, lab certificates, dosing clarity, and consent documents. Seek independent evidence and a written follow-up plan.
Can I combine therapy with a vacation?
Often yes, but recovery comes first. Time activities to avoid interfering with treatment or early healing.
Umbilical-cord vs. fat/bone marrow—what’s the difference?
Donor (cord) cells are readily available; autologous (fat/bone marrow) requires harvesting. Suitability depends on indication and patient factors—confirm with your specialist.
Are results permanent?
Durability varies by condition and protocol. Most non-transplant applications aim to reduce symptoms or improve function rather than cure disease.
Get Started with Stem Cell Therapy in Latin America
Latin America offers access to innovative non-transplant therapies at lower costs—if you pair opportunity with strong due diligence.
- Most uses beyond established indications are experimental
- Oversight and quality standards vary
- Marketing claims require verification
- Cell handling/processing quality is critical for safety
- Cross-border legal recourse is challenging
Do thorough research, ask direct questions, confirm credentials and lab standards, understand evidence and risks, and weigh potential benefits carefully.
Facilitators like Medical Tourism Packages can help evaluate options, coordinate logistics, and support informed decisions that put your safety first.